Colourfree Baby Drops 1-2 Months

Colourfree Suspension 1-5 Years

Chewable Tablets 3+

Suppositories 6 Months - 5 Years

Colourfree Suspension 5-12 Years

Elixir 5 - 12 Years

Suppositories 5-12 Years

Soluble 7+

Panadol Tablets

Panadol Caplets with Optizorb Formulation

Panadol Tablets with Optizorb Formulation

Panadol Gel Caps

Panadol Mini Caps

Panadol Suppositories

Panadol Back & Neck

Panadol Extra Caplets

Panadol Rapid Soluble

Panadol Rapid Caplets

Panado Rapid Handipak

Panadol Back & Neck Long Lasting

Panadol Osteo

Panadol Cold & Flu + Decongestant

Panadol Cold & Flu - Flu Strength (Day & Night)

Panadol Cold & Flu Relief + Cough

Panadol Cold & Flu MAX Hot Lemon
Compare Now (0/5)
- Product
- Format
- Age
- Key Features
- Ingredients


Colourfree Baby Drops 1-2 Months
- Concentrated Drops
- 1 Month - 2 Years
- Gentle on Tiny Tummies
- 500mg Paracetamol
- No gluten, lactose or sugar


Colourfree Suspension 1-5 Years
- Suspension
- 1-5 Years
- Strawberry/Orange Flavour
- Active Ingredient: Paracetamol 24 mg/mL


Chewable Tablets 3+
- Dissolvable Tablets
- 1-5 Years
- Perfect For Travel
- Active Ingredient: 120mg of Paracetamol per tablet


Suppositories 6 Months - 5 Years
- Suppositories
- 6 Months - 5 Years
- For vomiting
- Active ingredient: Paracetamol 125mg per suppository.


Colourfree Suspension 5-12 Years
- Suspension
- 5-12 Years
- Strawberry/Orange Flavour
- Active ingredient: Paracetamol 48 mg/mL


Elixir 5 - 12 Years
- Suspension
- 5-12 Years
- Fast & gentle relief
- Active ingredient: Paracetamol 48 mg/mL

Suppositories 5-12 Years
- Suppositories
- 5-12 Years
- For vomiting
- Active ingredient: 250mg Paracetamol per suppository


Soluble 7+
- Effervescent Tablets
- 7+ Years
- Absorbed quicker
- Active ingredient: Paracetamol


Panadol Tablets
- Tablets
- 12+ Years
- Basic Pain
- Active ingredient: 500mg Paracetamol


Panadol Caplets with Optizorb Formulation
- Caplets
- 12+ Years
- Quicker Absorbtion
- Active ingredient: 500mg Paracetamol


Panadol Tablets with Optizorb Formulation
- Tablets
- 12+ Years
- Quicker Absorbtion
- Active ingredient: 500mg Paracetamol


Panadol Gel Caps
- Caplets
- 12+ Years
- Easier to swallow
- Active ingredient: 500mg Paracetamol


Panadol Mini Caps
- Caplets
- 12+ Years
- Easier to swallow
- Active ingredient: 500mg Paracetamol


Panadol Suppositories
- Suppositories
- 12+ Years
- For vomiting
- Active ingredient: 500mg Paracetamol per suppository.


Panadol Back & Neck
- Caplets
- 12+ Years
- Fights Back Pain
- Active ingredient: 500mg Paracetamol


Panadol Extra Caplets
- Caplets
- 12+ Years
- Fight Tough Pai
- Active ingredient: 500mg Paracetamol , 65mg caffeine

Panadol Rapid Soluble
- Dissolvable Tablets
- 12+ Years
- Absorbed 2x Faster
- Active ingredient: 500mg Paracetamol


Panadol Rapid Caplets
- Caplets
- 12+ Years
- Absorbed 2x Faster
- Active ingredient: Paracetamol

Panado Rapid Handipak
- Caplets
- 12+ Years
- Absorbed 2x Faster
- Active ingredient: 500mg Paracetamol

Panadol Back & Neck Long Lasting
- Caplets
- 12+ Years
- Up to 8 hours
- Active ingredient: 655mg Paracetamol


Panadol Osteo
- Tablets
- 12+ Years
- Up to 8 hours
- Active ingredient: 665mg Paracetamol


Panadol Cold & Flu + Decongestant
- Caplets
- 12+ Years
- With Decongestant
- 500mg Paracetamol


Panadol Cold & Flu - Flu Strength (Day & Night)
- Caplets
- 12+ Years
- Day & Night Relief
- 500mg Paracetamol


Panadol Cold & Flu Relief + Cough
- Caplets
- 12+ Years
- Cough Relief
- 500mg Paracetamol
Minimise
Fever in Children
What is a fever?
A fever is an increase in your child’s body temperature. It is part of the body’s normal response to infections, and it plays an important role in fighting such infections. Your child’s temperature will return to normal when the infection has gone.

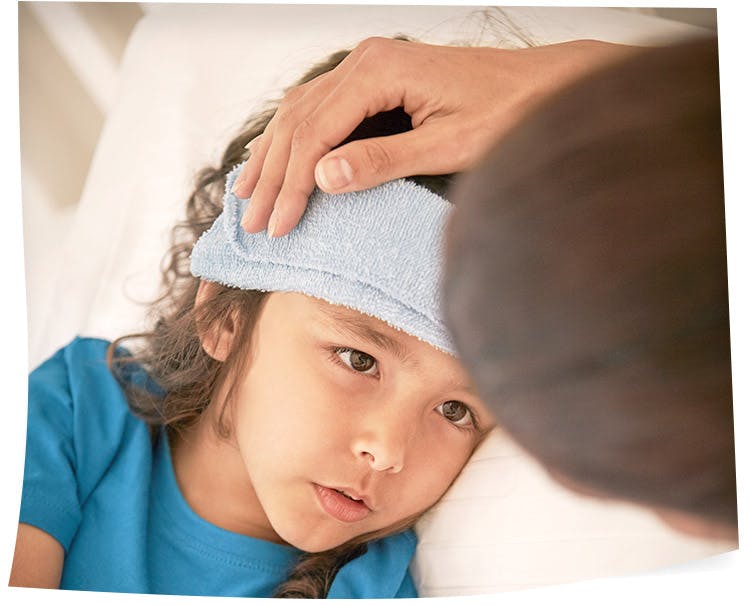

A child’s normal body temperature is 36.5°C–37.5°C when measured under their arm. A temperature of over 38°C indicates a fever.
A child’s normal body temperature is 36.5°C–37.5°C when measured under their arm. A temperature of over 38°C indicates a fever.
Fever in babies can be a sign of serious illness or infection. If your child is 3 months or under and has a fever of 38°C or above, or if your child seems very sick, they need to be seen by a doctor as soon as possible.
Types of thermometers
There are several different types of thermometers available. Your doctor or pharmacist will be able to offer you advice. Always follow the instructions that come with the thermometer.
Digital thermometers:
These are easy to use and beep when they’re ready. Some also bend to mould into the shape of a child’s underarm. Taking your child's temperature under the arm is recommended as the easiest and safest method for young children, but may be up to 1°C lower than temperatures measured by mouth (a method suitable only for older cildren).
Infrared thermometers:
These are quicker (almost instantaneous) and easier to use and read, but more expensive. There are two types:
- Those inserted in their ear – these can be useful for older children but are not suitable for newborns as their ears are so small.
- Those held up against their temple (non-contact). An advantage of these is that you can use them while your child is asleep, although they may be inaccurate.
Do not sponge your child with water – this does not help to reduce a fever.
What else can you do when your child has a fever?
- Depending on your child’s age and symptoms, you can give them a temperature-lowering medicine such as paracetamol (See ‘Using medicine’).
- Offer your child regular drinks (where a baby is breastfed, the most appropriate fluid is breast milk).
- Look for signs of dehydration – sunken fontanel (soft spot on a baby’s head), dry mouth, sunken eyes, no tears, and fewer wet nappies than normal. If your baby has signs of dehydration, take them to hospital immediately.
- Do not under or over dress your child. If they are shivering or sweating a lot add more or less clothing accordingly.
- Sponging your child with luke-warm or cold water is not recommended.
- Check your child regularly for rashes and to see if they are getting better. If a rash appears or if you are concerned that your child is not improving, contact your doctor for advice.
- If your child attends daycare, it’s best to keep them at home while they have a fever and notify the daycare centre of the illness.
When to contact your doctor
You should see a doctor if your child has a fever and any of the following:
- the child is younger than 3 months
- the fever persists for more than 24 hours.
- the fever doesn’t respond to paracetamol.
- the child refuses to drink or wees less often (indicating possible dehydration).
- they have an earache.
- they keep vomiting or have frequent bouts of diarrhoea.
- they are very pale or weak.
- they are unusually sleepy or drowsy.
- they complain of a stiff neck, persistent headache or light hurting their eyes.
- they are screaming, very irritable and unable to be consoled.
- you are concerned for any other reason.
When it is an emergency
You should take your child to hospital or call 000 for an ambulance if:
- they have severe vomiting and can’t keep down any fluids.
- they have difficulty swallowing.
- they have fast breathing or difficulty breathing.
- they have a bulging fontanel (the soft spot on the head in babies).
- they are having fits or convulsions (jerky, uncontrollable movements).
- they are unconscious (you can’t wake them up).
- they have a fever and their neck seems very stiff or rigid.
- they have a fever together with a rash.
.png?auto=format)
Febrile convulsions
A febrile convulsion is a fit or seizure that occurs in some children when they have a high fever.
Most children with fever suffer only minor discomfort. However 1 in 30 will have a febrile convulsion at one time or another. This usually happens between the ages of 6 months and 6 years. Most children with febrile convulsions only ever have one fit. Febrile convulsions are not harmful; they do not cause brain damage or epilepsy.
Most children with fever suffer only minor discomfort. However 1 in 30 will have a febrile convulsion at one time or another.
What happens during a febrile convulsion?
During a febrile convulsion your child usually loses consciousness, their muscles may stiffen or jerk and they may also have difficulty breathing and go red or blue in the face. When the movements stop, your child will regain consciousness but remain sleepy or irritated afterwards.
Febrile convulsions are quite upsetting for parents to witness. Remember, most seizures will stop within seconds or a couple of minutes without any medical treatment.
What can you do during a convulsion?
- The most important thing is to stay calm.
- Place your child on a soft surface, lying on their side.
- Do not put anything in their mouth – your child will not choke or swallow their tongue.
- Try to watch exactly what happens, so that you can describe it later.
- If possible, time how long the convulsion lasts.
Call an ambulance on 000 if:
- you feel worried.
- it’s your child’s first convulsion.
- the convulsion lasts more than 5 minutes.
- your child’s breathing doesn’t return to normal after the convulsion.
- your child does not wake up when the convulsion stops.
- your child looks very sick when the convulsion stops.
- your child was very unwell before the convulsion started.
- you are concerned for any other reason.
Key points to remember
- Approximately 3% of children between the ages of 6 months and 6 years have a febrile convulsion at one time or another.
- Nothing can be done to prevent the convulsion from occurring. Remain calm and try not to panic.
- Never put a child in a bath (to lower their temperature) during a convulsion.
- Febrile convulsions will not cause brain damage. Even very long convulsions lasting an hour or more almost never cause harm.
- If your child has a convulsion, and you haven’t taken them to hospital, make an appointment to see your doctor.
Reference
Sydney Children’s Hospital Network [Accessed Dec 2014].
Available from: www.schn.health.nsw.gov.au/parents-and-carers/fact-sheets/fever